-
Medical Innovation
Artificial Pancreas Keeps Patients Healthier: A Perspective
The late Mayo endocrinologists Russell Wilder, M.D., and Randall Sprague, M.D., would be smiling today at the news for patients with diabetes. Much of their lives and careers were dedicated to making sure Type 1 diabetes patients received the right amount of insulin at the right time to live long, healthy lives. I'm referring to the recent study in The New England Journal of Medicine demonstrating that an artificial pancreas — a closed-loop system of insulin pump and feedback monitor — is better at keeping patients in their glycemic range than current systems.
Mayo researchers were among those at seven institutions whose work was represented in this six-month randomized clinical trial. The conclusion is straightforward: Using a system that employs an algorithm-guided, computerized feedback loop to provide a constant and adjusted flow of insulin provides better control than a sensor-augmented pump. In other words, the artificial pancreas did a better job keeping the participants' blood sugar levels in the normal or near normal range during the time of the study. Constant measurement, feedback and adjustment of insulin volumes, including boluses of the drug when needed, happens automatically.

"Patients with Type I diabetes will move to new technologies when they are confident that the technology is dependable and an improvement on their current reliable system," says Yogish Kudva, M.B.B.S., Mayo physician-researcher and paper co-author. "This nationwide study, supported by the National Institutes of Health, validates the value of a closed-loop system."
A cohort of 168 people participated in the study across these seven institutions:
- Barbara Davis Center for Childhood Diabetes at University of Colorado Anschutz Medical Campus
- Icahn School of Medicine at Mount Sinai
- Joslin Diabetes Center
- Mayo Clinic
- Sansum Diabetes Research Institute
- Stanford University
- University of Virginia
Of those, 112 were assigned to using the closed-loop technology and 56 were in the control group, using a regular insulin pump. The percentage of time that the closed-loop group was in the target range for blood sugar levels increased over the six months and showed a difference of 11 percentage points, compared to the control group.

This device, still awaiting Food and Drug Administration approval, would be the second such system after the Medtronic 670G system, which has been available in the U.S. since March 2016.
Discovery's Edge reported on early studies on Mayo's closed-loop system in 2012, and this writer recalls a news release about findings presented at the American Diabetes Association in summer 2011. It was, as always, team science — collaborative research with Mayo and external colleagues. The mathematical modeling came from Italy and led to an artificial pancreas algorithm.
The current study uses an algorithm pioneered by Boris Kovatchev, Ph.D., at the University of Virginia. This work mirrors the earliest days when Mayo was part of an ad hoc group of expert centers conducting early clinical trials on insulin. That group of five to seven hospitals were asked by the discoverers of the drug — Drs. Banting and McLeod of Canada — to research and publish safe dosages of insulin for varying types of patients. Much of this work was published in and just after 1923. The Mayo team was led by Dr. Wilder, who began studying children with diabetes mellitus Type 1 soon after his arrival in Rochester, Minnesota, in 1919. Over the ensuing century, four generations of Mayo researchers and a long list of collaborative publications have bridged the time when Type 1 diabetes patients rarely survived to adulthood to today's engineering advancements.

I should explain about Dr. Sprague. As a young boy, he was one of the first patients to be saved by the introduction of insulin, which was prepared at his physician's office in Chicago from animal glands. He grew up to become an endocrinologist and researcher, and arrived at Mayo Clinic in time to be mentored by Dr. Wilder. He published his own research and commentaries in medical journals well into the 1980s.
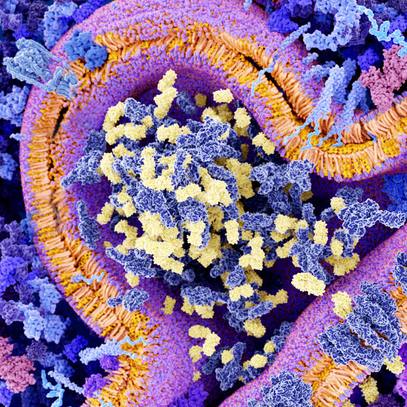
A search of Mayo research over the past dozen years shows just under 900 articles on diabetes of some type, nearly 70 in this year alone. The research continues at the molecular and cellular levels; in transplant and regeneration of pancreatic tissue; as well as ongoing clinical studies, including related conditions, such as obesity and metabolic syndrome.
— Bob Nellis, December 2019